'Too few consequences' for NHS underperformance - Miles
 Getty Images
Getty ImagesThere are "too few consequences" for underperformance in the NHS, Wales' health secretary has said.
Outlining plans to reduce waiting lists to health leaders on Monday, Jeremy Miles said proposals included putting patients who miss outpatient hospitals at the back of the queue.
Other potential changes include encouraging patients to get "fit for surgery", commissioning some private health care at a national level and reform among NHS leadership.
The proposals have been welcomed by some patients and hospital workers, but a health equality charity said the changes could lead to people delaying seeking help
The proposed changes are part of a number of Welsh government ideas being discussed to improve the NHS, which has recently seen small reductions in record waiting lists.
"On too many occasions, I have been met with the equivalent of a shrugging of shoulders when I've challenged people on why a budget has been blown or a target not met," said Miles.
He said consequences are needed among patients who repeatedly miss outpatient appointments, or cancel at the last minute, though the vulnerable and children would be protected.
Miles also proposed the commissioning of some private health care at a national level to enable a more strategic approach.
Greater regional collaboration is needed to help drive down waiting times, according to the health secretary, while reform at the top level of leadership should be refocused to provide better support and allow the Welsh government to "hold the service to account".
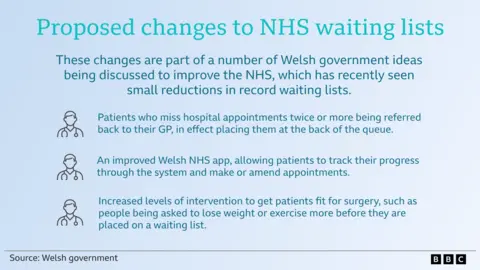
The Welsh government said patients who were fit and well before surgery were more likely to recover quickly and support would be given to get them "in the best possible shape" for treatment.
But health equality charity Fair Treatment for the Women of Wales (FTWW) said "fear of weight stigma" could delay some people from seeking help.
Sioned Rees, 47, from Pen-y-groes in Carmarthenshire recently lost 11 and a half stone after she was advised by medical professionals to lose weight.
"[I was] told for most of my life that I needed to lose weight when I went to see the doctor," she said, "but the right intervention wasn't there".
"I definitely agree that people need to take control of their health but they do need help.
"It's not just a simple statement, 'you need to be fitter before you can have the operation'."
 Sioned Rees
Sioned ReesMiles said 700,000 hospital outpatient appointments were missed or cancelled last year. On average this equates to about 2,700 every working day.
He said patients should do more to improve their own health "to make the best possible use of scarce NHS resources".
But FTWW raised concerns that blanket processes risked inadvertently penalising those who experienced "barriers not of their own making" and called for engagement with "diverse patient communities".
They said one of the biggest issues reported by members was an inability to get hold of someone to cancel or reschedule appointments.
"We know, for example, that women in particular are more likely to be primary care givers in Wales, so appointments which are made without first establishing other responsibilities and commitments can be problematic."
 Getty Images
Getty ImagesHospital volunteer John Timmons, 70, said he saw "a ridiculous number" of patients not turning up for appointments and would support the plans.
"Somebody else that's desperate could be there - if they're working age, they could get themselves back out to work," said Mr Timmons, from Cardiff.
He was referred by his physiotherapist to an exercise scheme at his local leisure centre to help him during the wait for his second knee replacement.
"Being fit definitely helps with recovery," said Mr Timmons, who added he had also experienced social benefits from exercise.

Annie Hillman is a community sport and health manager for the eight Better Leisure Centres across Cardiff.
The centres have co-delivered sessions with the NHS for several years, where patients with hip, knee and back pain can self-refer, or be referred by hospital physiotherapy teams.
NHS staff then deliver classes at the leisure centre instead of the hospital setting.
The centre's own staff have also been trained to take sessions or assess patients referred by their GP.

"At the end of the six week programme where they would have left the hospital setting they're already in the leisure centre, they've already broken down that barrier of coming through the door," she said.
"They see people like themselves exercising, and that is the change of behaviour that they continue to have. It's prevention - they don't want to go back to the doctors, they don't want to go back to the NHS, they keep active.
"There's a huge demand but the lack of funding for us is a problem."
It is a resource she wishes she had when a spinal injury caused her to have surgery in 2009.
"I had to learn to walk again," said the 53-year-old former Wales netball player.
"I came out of hospital and was in a bit of a dark place. There was nothing like this going on where I could meet people who had gone through the same thing."

Paul O'Sullivan retired 10 months ago and has filled his days with sessions at the leisure centre, after also being referred by his physiotherapist following a second knee replacement six months ago.
"My wife is here having been referred by a pharmacist for osteoarthritis in the hip - she loves it and comes for five hours a week," he said.
The 70-year-old said he would support "a patient deal" where there is a greater expectation on people to remain active.
"I didn't know what to do with my first knee two years ago, with the second I was back here after six weeks, because I'd done a lot of classes pre-op and I knew what to expect.
"It made a massive difference."
He acknowledged it would not be as straightforward for everyone and said those missing appointments may have valid reasons.
"It's about education, because it does cost money when you miss an appointment and extends the waiting list."