Ambulance patient waits 19 hours outside hospital
 PA Media
PA MediaA patient has waited 19 hours in the back of an ambulance outside a hospital's emergency department, the medical director of the Northern Ireland Ambulance Service (NIAS) has said.
Dr Nigel Ruddell told BBC News NI it was caused by "sustained and extreme pressure".
He said that ambulance crews are currently facing lengthy delays handing patients over to hospitals because of a "lack of flow" in the system.
This has been caused by a spike in respiratory illnesses and difficulties in discharging hospital patients back home, he added.
"Our crews are effectively stuck outside (emergency departments)," Dr Ruddell said.
He told the BBC's Good Morning Ulster programme that he had "just heard this morning of somebody waiting 19 hours to be handed over".
The NIAS said it would not be providing any further comment.
Dr Ruddell added: "There is no doubt we are facing a period of really sustained extreme pressure primarily due to large numbers of patients presenting with respiratory illness particularly affecting all hospital sites over the past week.
"This coupled with challenges discharging patients back home or to the community effectively causes stagnation.
"It is causing very significant delays in being able to hand over our patients when we arrive to emergency departments," he said.

The NIAS said it was "experiencing severe challenges" as a result of the pressures being felt across the system, while the Department of Health said that the healthcare system was working extremely hard to care for patients while under "severe pressure".
On Monday, Dr Michael Perry, vice chair of the Royal College of Emergency Medicine in Northern Ireland, told BBC News NI no patient should have to wait anything like 19 hours to be transferred to hospital from an ambulance.
"It is completely unacceptable, I don't think any clinician would think this is acceptable," he said.
"The sad fact is this is not uncommon, it's our opinion it is becoming more common."
He said patients were being left in ambulances because "we simply don't have any room to offload ambulances into emergency departments".
Winter has only exacerbated already existing pressures in the health system, Dr Perry added.
"The reality is that we have been in the hundreds of patients waiting for beds in our hospitals for the last number of months.
"We have had the very predictable rise in the cases of flu, Covid and winter vomiting bug, which are all predictable… but the system is just under immense strain and pressure."
Dr Perry said staff morale is "extremely low".
"We do not see a light at the end of the tunnel," he added.
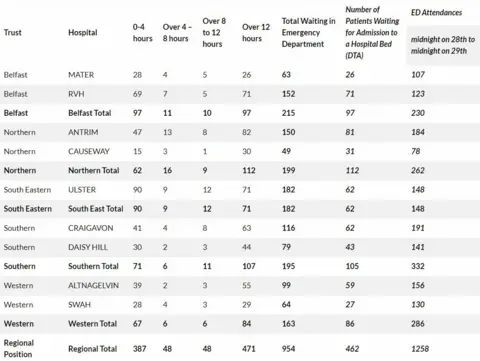
According to the latest Department of Health (DoH) data on Monday, across a 24-hour period from midnight on Saturday to midnight on Sunday, 1,258 people attended emergency departments (EDs) across Northern Ireland - with 954 waiting to be seen and 462 queuing for a bed.
The busiest area across Northern Ireland was the Southern Trust, where more than 332 people attended emergency departments and 105 had to wait for a bed.
 DoH
DoHWinter planning
Meanwhile, Rita Devlin of the Royal College of Nursing said winter needs to be planned for well in advance.
"We need more district nurses, more acute care at home teams, we need to think differently, to do things differently, we need to realise we can't keep doing the same thing," she said.
 PA Media
PA MediaLast month, Health Minister Mike Nesbitt announced a Winter Preparedness Plan, which includes additional funding for GP and residential care homes, phone first services for all trusts, and vaccination programmes.
"The planning process for winter gets underway in springtime, to ensure that we can mitigate, as far as possible, the additional pressures that we know we will face," he said.
'We have to change our system'
Speaking to BBC Radio Foyle's North West Today programme on Monday, Dr Alan Stout from the BMA said systemic change was needed.
"Winter will always bring additional pressures particularly when we get high levels of circulating infection as we do at the moment, that is always going to be exceptionally difficult to deal with," he said.
"But the reality is we have a health service that is dealing with winter pressures year round at the moment … we have to change our system, change the way we do things, the way we deal with patients," he said.
