Long waits outside EDs causing deaths - ambulance chief
 BBC
BBCDelays getting patients into emergency departments (EDs) is leading to an increase in deaths, the medical director of the Northern Ireland Ambulance Service (NIAS) has said.
Dr Nigel Ruddell said the longer patients wait outside an ED the more they are likely to deteriorate.
Last week, the deputy chair of the British Medical Association in Northern Ireland said EDs were at breaking point.
Nineteen of the Northern Ireland Ambulance Service's 56 crews were waiting with patients outside emergency departments early on Friday morning.
Speaking to BBC Radio Ulster's Good Morning Ulster programme, Dr Nigel Ruddell said there was a "slow down in the flow of patients right through the system".
"There is no doubt that the pressures of the system are causing risk to patients and we're working hard to try and balance that risk.
"Both ourselves in the ambulance service and our colleagues in hospitals recognise that this inability to get patients in, assess them and treat them quickly is causing harm, and the evidence would show that does cause a rise in increased deaths."
One ED consultant at the Royal Victoria Hospital in Belfast said earlier this week that it was disgraceful that corridor care in emergency medicine had become "almost normalised".
Another said that until social care was addressed in Northern Ireland, the predictable Christmas spike would not change.
Dr Ruddell added that the delays were "incredibly frustrating" and "increases the risk" to patients.
"That's not just the most critical calls for people who have collapsed with cardiac arrests etc, people with chest infections, abdominal pain, injuries etc, the longer the wait for an ambulance the more risk they carry."

"Sitting waiting with patients hearing other emergency calls coming in is very challenging for crews out on the ground and for all the staff in the control room who are desperate to respond to patients as quickly as possible," Dr Ruddell said.
'The system is beyond repair'

Johnny Hanna is a paramedic who started his shift at 07:30 GMT on Friday and was immediately dispatched to the Ulster Hospital to relieve a crew who had been sitting outside the ED since 04:00.
They were with a patient who had fallen at 14:00 on Thursday and was eventually admitted to the hospital at 10:15 on Friday.
Mr Hanna said the "normality now is to go up to hospitals to relieve crews to let them go home".
"It's placing crews and patients at a detriment sitting here, crews aren't receiving their meal breaks or getting home on time. It's putting pressure on their family life and their mental health," he said.
"We do this job to help people in the community, we don't come up here to sit and basically babysit patients in 'yellow cubicles', as we know them as now. It's not fair on anybody, the system is just beyond repair now."
Mr Hanna added that ambulances are not designed to be sat in for long periods of time but rather "to get patients from A to B as quick as possible".
"They're uncomfortable, at times they're very cold, stretchers aren't made for patients to be lying on for 6, 7, 8 hours a day.
"It's not right, we do our best to comfort and care for the patients, we provide them with tea and coffee but it's third world standards, it's unacceptable but we're just doing our best."
How many people are waiting in EDs?
The latest figures show that there were 649 people in EDs on Friday morning with 190 waiting more than 12 hours.
The numbers waiting for a hospital bed have dropped from about 350 to 279.
BBC News NI was told on Monday that one patient with flu was being treated in an unused tea room in the Royal Victoria Hospital in Belfast (RVH) while three others had been in the same area for four days.
At 17:00 GMT on Monday, 1,052 people were in Northern Ireland's nine EDs.
A lead nurse said staff were "treating the most vulnerable, elderly sick patients in an intolerable environment".
The combination of a cold snap and flu season have been seen as major factors driving the crunch at emergency departments.
A lack of care packages in the community has also preventing hospitals from discharging patients and opening up bed space.
More than 500 people considered medically fit were unable to be sent home from Northern Ireland's hospitals on Sunday night.
Earlier this week, a Belfast Health Trust spokesperson said that was not how the trust wants to treat emergency patients.
The Department of Health said longer-term solutions required sustained investment and reform.
At an emergency meeting on Tuesday, Northern Ireland's health minister said "pressures are both serious and nationwide" and that patients often have to surrender "their dignity and their privacy".
Mike Nesbitt announced that flu vaccines, currently available for free to those aged 65 and over, would be extended to the 50-64 age group.
Pressures on ambulance service
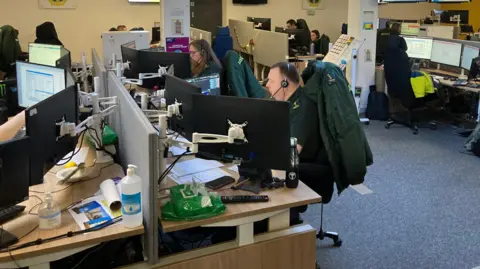
Aileen Moynagh, health reporter at ambulance control
This control room is the first point of contact for the public anywhere in Northern Ireland phoning 999, seeking immediate medical care.
When I arrived at 07:30 it was a calm enough picture.
At that stage, out of 56 ambulances starting, 19 were sitting outside hospitals across Northern Ireland.
The longest one had been waiting from 22:19 on Thursday.
Staff said that has a knock-on affect on crews - it means later finishes for one crew and later starts for those on the incoming shift.
Within about 45 minutes, the ambulance back up had reduced from 19 to 12 vehicles.
At 08:45, four more ambulances cleared, although there were four more ambulances on their way with patients.
It was a very moving and very changeable picture.
And taking a snapshot at any given time doesn't give a trust picture of the day.
Staff told me that pressures tend to ease on Fridays ahead of the weekend, but then pick up again, particularly heading into a Monday.