Experts encouraged by new prostate cancer test
 BBC
BBCResearchers say they have been encouraged by trials of a new process to detect prostate cancer in men.
It is hoped that the approach, developed at Heriot Watt University in Edinburgh, could lead to quicker diagnosis and earlier preventative treatment.
Prostate cancer is the most common cancer for men in the UK, with one in eight diagnosed with the disease in their lifetime.
The process uses existing ultrasound equipment which is widely available in most hospitals, instead of expensive MRI scanners which can have long waiting lists and result in delays to treatment.
The test involves injecting a solution containing millions of tiny, harmless microbubbles into a vein.
These bubbles travel through the patient's bloodstream to the prostate and are tracked using ultrasound technology.
The altered blood flow in cancerous tissue is highlighted by the solution and shows up on the ultrasound scan.
Research scientists at the university, working alongside doctors at the Western General Hospital in Edinburgh, have completed early-stage clinical trials.
They say that the signs are "extremely encouraging", with a 94% detection rate of prostate tumours.
The trials are set to continue - although realistically it could be between three and five years before the technique can be used in a clinical setting.
Professor Alan McNeill, a consultant urological surgeon at the Western General Hospital, said the initial trial results provided useful information for the diagnosis and treatment of prostate cancer.
He said: "The technology has the potential to significantly enhance diagnostic accuracy, help clinicians like me to carry out more targeted biopsies, and even focus treatments with greater precision.
"I can anticipate it benefiting treatments like focal therapy by allowing us to pinpoint and treat cancerous tissue with greater accuracy.
"Nearly every week, my colleagues and I meet men in their 50s or early 60s suffering from advanced prostate cancer that leaves them with fewer treatment options."
 Getty Images
Getty ImagesProfessor Vassilis Sboros from Heriot-Watt University is co-founder of Less Grey Imaging.
He says the technology can help support an NHS fit for the future.
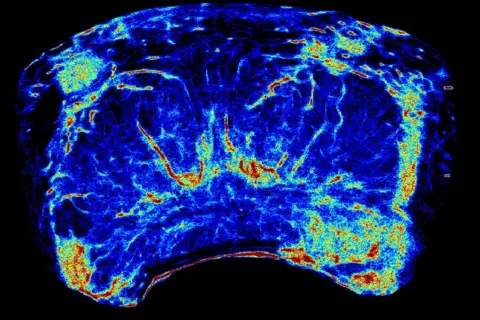
"By utilising existing ultrasound scanners found in hospitals and clinics worldwide, we're able to produce high resolution images of the prostate that clinicians have never seen before.
"With one man dying from prostate cancer every 45 minutes in the UK, we hope earlier detection will radically improve treatment outcomes, saving lives while reducing the number of people sent for unnecessary and often risky tests."
Prostate cancer is not always life-threatening and can be cured if it is caught early enough.
There is no prostate cancer screening programme in the UK, unlike those for breast, bowel and cervical cancer.
Instead, the onus is on men to request a prostate specific antigen (PSA) blood test from their GP once they are over 50.
These PSA tests are then used to decide whether or not a patient needs to go for an MRI scan.
Last year six-time Olympic cycling champion Sir Chris Hoy called for a review of prostate cancer testing following his own terminal diagnosis.
Hoy announced in August last year that he had been diagnosed with primary cancer in his prostate and could have between two and four years to live.

Gary Tait, 61, from Edinburgh was treated for prostate cancer five years ago after his wife, a practice nurse, encouraged him to see his GP.
He now chairs the Edinburgh and Lothian prostate cancer support group - which fully supports the development of the new technology.
Mr Tait says the new test raises the possibility of men being diagnosed and treated earlier.
He said: "Being diagnosed and treated for prostate cancer is an incredibly anxious time so it is very positive to see these trial results which indicate that the new ultrasound technique could lead to more accurate diagnosis of prostate cancer.
"From the perspective of men who are unaware of a developing tumour in their prostate, this improved method of diagnosis could lead to earlier treatment which improves the likelihood of a good outcome."
