Living hell for 'forgotten' skin patients
 BBC
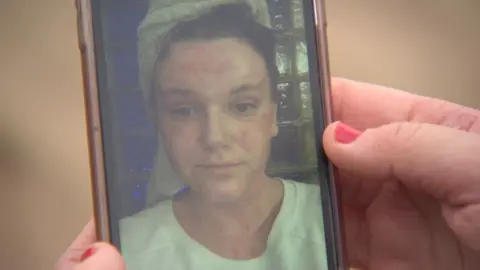
BBC"It's taken a big toll on my life," says Elle Jones, 19, reflecting on her severe eczema.
The office worker from Devon describes days bedridden with "excruciating" pain and chronic itching, while waiting up to 18 months for NHS treatments.
But she says the emotional impact is the worst part, making her feel "trapped, hopeless" and afraid of never being "free" from her skin disease.
Miss Jones is one of thousands of people across the country who are waiting a year or more to see a dermatologist due to pressure on services caused by increased urgent skin cancer referrals and a shortage of specialist doctors.
"I've missed out on work, school, college," says Miss Jones, adding she has "spent a long time hating myself".
 Elle Jones
Elle JonesOne in 10 people in the UK has eczema and one in five children, according to the National Eczema Society.
It is often lifelong and incurable.
Miss Jones says her life got "dark" when she experienced a severe flare-up at college in 2021, describing it as a "never-ending tunnel because there's just no light there".
"You're stuck in pain and agony," she says.
"Your skin is always red... bleeding all the time... I couldn't even recognise myself.
"It's soul-destroying."
She says steroid and moisturiser creams prescribed by her GP "just made me burn and itch", so she was referred to see a dermatologist.
However, 12 months later she was still waiting, when she moved home to Devon from college.
She then waited a further 12 months for light therapy, and 18 months at the same time for skin allergy patch testing in summer 2024.
 Elle Jones / BBC
Elle Jones / BBCPatch testing results showed several skin reactions, so she cut out make up, hair and nail products, but nothing helped.
The longest wait for dermatology treatment in her area in north Devon is two years, according to NHS data published for January, with overall waits in the country longer than the England average.
Miss Jones is now trying an immunosuppressant drug which she says makes her "sleep all weekend".
Her hunt for successful treatment continues.
She says she has learned to accept her condition, stay positive and "keep fighting".
'The forgotten many'
Inflammatory skin disease patients often face long waits because departments are inundated with growing skin cancer referrals, which are the highest of any NHS urgent cancer referrals.
These diagnoses are prioritised, with waiting time targets set by the government.
Coupled with that, a shortage of dermatologists is adding pressure.
Some patients also report long waits for non-life threatening skin cancer treatments and follow-ups.
Waiting times to receive treatment across NHS dermatology departments in England are longer than they were before the Covid-19 pandemic.
NHS data from the beginning of the year, shows 43% of patients waited longer than the NHS target of 18 weeks at the start of 2025.
About 9,000 people had been waiting for one year or more.
 Patient handout
Patient handoutThree of the most common inflammatory skin diseases are eczema, psoriasis and acne, which can cause permanent scarring.
Some patients try treatments through their GP for years before being referred to a consultant and some are admitted to hospital with repeated infections.
Consultant dermatologist Dr Toby Nelson who practises in Cornwall and Devon, describes these patients as "the forgotten many".
He says: "You can't say skin cancer shouldn't take priority over these other patients, but at the moment there does seem to be a significant imbalance.
"Some are in a living hell."
Dr Nelson says more are turning to private healthcare to be seen quickly.
But some of them face further disappointment, as newer "transformative medicines" can only be prescribed by the NHS, he adds.
He advises people on waiting lists to make healthy life choices with things like sleep, alcohol and smoking "as skin disease is rarely just related to the skin".
"In some situations this will improve your skin disease on its own," he says.
 Ben Varco
Ben VarcoLike Miss Jones, Ben Varco, 24, from St Austell in Cornwall has been suffering behind closed doors.
"It's draining both mentally and physically," he says.
"You feel embarrassed to go out."
Mr Varco, a wine cellar worker, says he was referred to dermatology on the NHS in July 2024 for severe acne but nine months later has heard nothing.
"I feel kind of ignored, like it's not really taken seriously," he says.
Private care has cost him more than £1,000 to date.
Liam Garner, 19, sought private treatment following a severe eczema flare up in 2024.
The teaching assistant from Cornwall says: "I get it all over – the itch leads to bleeding... Moving can hurt and it keeps me up at night.
"I was off work for two months and had horrible anxiety."
Both young men needed help from their families to pay for treatment.
 Patient handout
Patient handoutSkin disease can also affect patients' mental health with 98% of those surveyed for the All Party Parliamentary Group on Skin's 2020 report saying it affects their emotional and psychological wellbeing.
Andrew Proctor, chief executive of the National Eczema Society, says: "We don't understand why people with eczema and other inflammatory skin conditions are being treated as second-class citizens by the NHS."
'Workforce shortage'
In September 2024 a British Association of Dermatologists (BAD) workforce report warned of a "particularly concerning" situation for dermatology services, stating: "It is clear that demand for our services is outstripping the capacity of our workforce to deliver care."
Meanwhile a benchmark NHS dermatology report in 2021 highlighted a "severe workforce shortage caused by a long-term restriction on the number of new dermatology training posts".
 Maia Gray/@its_just_acne
Maia Gray/@its_just_acneA Department of Health and Social Care spokesperson says the NHS is "broken and it is unacceptable that patients have been left waiting in pain".
They say it has delivered an extra two million appointments sooner than planned, and some of those were in dermatology.
The spokesperson adds the department will publish workforce plans this summer - to ensure the NHS can deliver the care patients need.
A spokesperson for the Royal Devon University Healthcare NHS Foundation Trust says it is difficult to recruit and it faces pressure from some of the highest skin cancer rates in the UK.
"We are working to transform the way we deliver care to reduce our waiting lists," they add.
'Super clinic'
Dr Carolyn Charman, clinical vice-president of BAD says the NHS must build on innovative skin cancer diagnostic schemes, which are key to relieving pressure.
She says there are "real opportunities to counteract the challenges" using digital technology, patient images and artificial intelligence.
She adds patients who are suffering while waiting should contact their hospital team and seek advice from reliable sources online such as BAD's website.
At the Royal Cornwall Hospitals Trust, patients like Mr Garner and Mr Varco wait for up to 12 months routinely, despite a raft of new measures.
A spokesperson says: "We have implemented many innovations to proactively respond to the increasing demand."
These include "super clinics" where one specialist supervises multiple resident doctors and specialist nurses and a community imaging service run by healthcare assistants.
 Katie Mackie/@mackies_moments
Katie Mackie/@mackies_momentsSome patients are using social media to help each other cope.
Katie Mackie, 28, and Maia Gray, 30, are "skin positivity influencers" from London.
Miss Mackie campaigns for charity Changing Faces after a "mentally draining rollercoaster ride" with eczema and wants others to know "things do improve".
"Tell people what you're going through, don't isolate yourself," she says.
"There is also free therapy and charities who can offer support."
Miss Gray who has had acne for 17 years, adds: "I think it needs to be highlighted that loads of people are struggling mentally with this.
"My message is whatever your skin condition is, continue to live life."
Follow BBC Cornwall on X, Facebook and Instagram. Follow BBC Devon on X, Facebook and Instagram. Send your story ideas to [email protected].
Get our flagship newsletter with all the headlines you need to start the day. Sign up here.